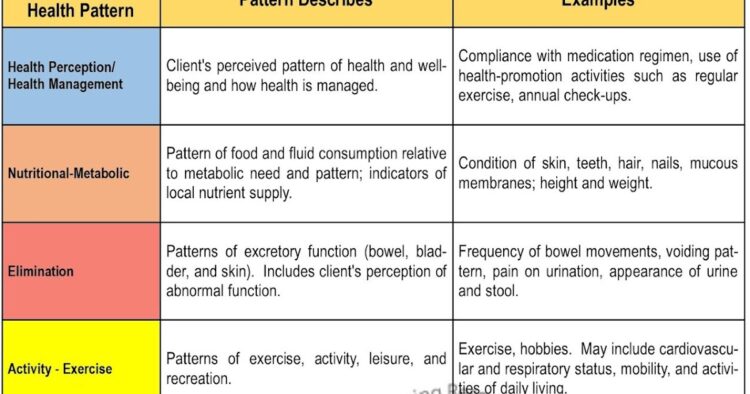
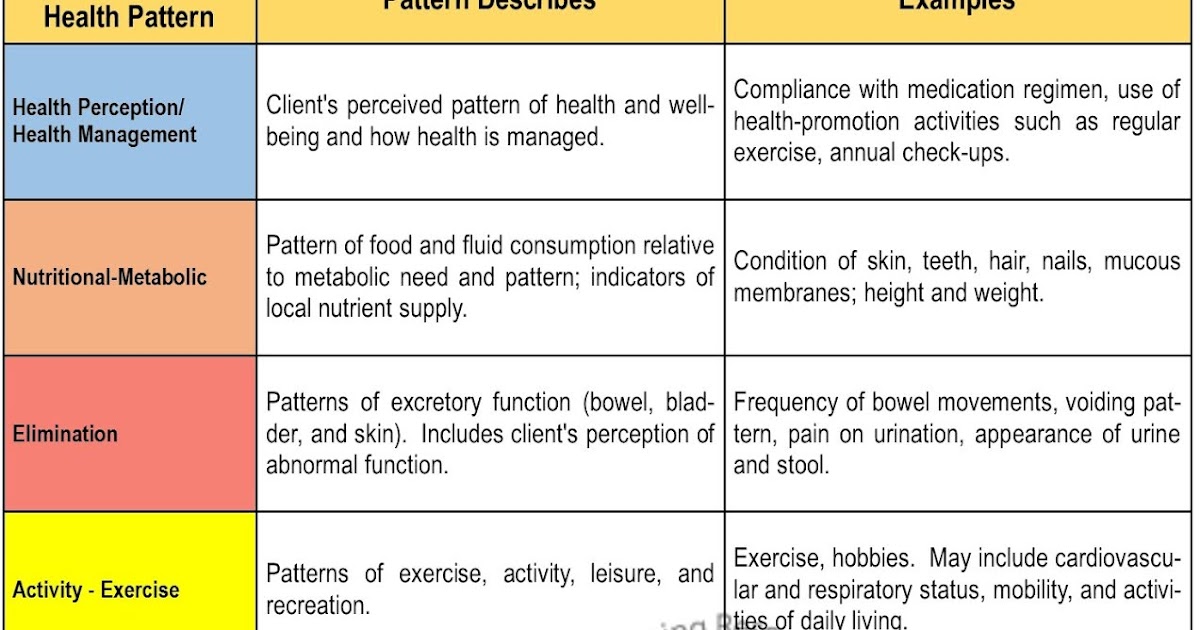
Assessment of Gordon Functional Health Patterns
Gordon Functional Health Patterns (FHPs) are a comprehensive framework for assessing the health status of individuals across various aspects of their lives. These patterns provide a holistic view of an individual’s well-being, encompassing physical, psychological, social, and spiritual dimensions.
To effectively assess each FHP, various methods and techniques are employed. These include:
Health History
A thorough health history is essential for gathering information about an individual’s past and present health status. It involves questions about medical conditions, hospitalizations, surgeries, medications, allergies, lifestyle habits, and family history.
Physical Examination
A physical examination provides valuable insights into an individual’s physical health. It includes assessments of vital signs, body measurements, skin condition, musculoskeletal system, neurological function, and other relevant parameters.
Mental Status Examination
A mental status examination assesses an individual’s cognitive, emotional, and behavioral functioning. It includes observations of appearance, speech, mood, affect, thought processes, and memory.
Functional Assessment
Functional assessments evaluate an individual’s ability to perform daily activities, such as self-care, mobility, and communication. These assessments help identify areas where an individual may require assistance or support.
Environmental Assessment
An environmental assessment examines the physical, social, and cultural factors that influence an individual’s health. It includes assessments of housing, neighborhood safety, access to healthcare, and social support systems.
Spiritual Assessment
A spiritual assessment explores an individual’s beliefs, values, and sense of purpose. It helps identify sources of meaning, hope, and resilience that can contribute to overall well-being.
Interpretation of Gordon Functional Health Patterns
Interpreting the findings of a Gordon Functional Health Patterns (FHPs) assessment is crucial for healthcare professionals to gain a comprehensive understanding of a patient’s health status and identify potential areas of concern.
FHPs provide a structured framework for assessing an individual’s health patterns across 11 key areas. By examining the patterns of responses, healthcare professionals can identify deviations from normal or expected responses, which may indicate underlying health problems or risks.
Identifying Potential Health Problems and Risks
The interpretation of FHPs involves identifying patterns and trends in the responses provided by the patient. For instance, a patient who reports difficulty sleeping, low energy levels, and poor appetite may be experiencing symptoms of depression or another underlying medical condition.
By recognizing these patterns, healthcare professionals can initiate further investigations, such as ordering diagnostic tests or referring the patient to a specialist, to determine the root cause of the patient’s symptoms and develop appropriate treatment plans.
Additionally, FHPs can help identify individuals who are at risk for developing certain health conditions. For example, a patient with a family history of heart disease who reports high cholesterol levels and a sedentary lifestyle may be at an increased risk of developing cardiovascular disease.
By identifying these risks early on, healthcare professionals can implement preventive measures, such as lifestyle modifications or medication, to reduce the likelihood of future health problems.
Nursing Interventions Based on Gordon Functional Health Patterns
Nurses play a pivotal role in using Gordon Functional Health Patterns (FHPs) to enhance patient care. By assessing each pattern, nurses can identify areas of concern and develop tailored interventions to promote health and well-being.
Interventions Tailored to Specific FHPs
Specific nursing interventions can be tailored to address the unique needs of each FHP:
- Health Perception-Health Management: Assess the patient’s perception of health, knowledge of health practices, and ability to manage health conditions. Interventions may include providing health education, promoting self-care, and supporting adherence to treatment plans.
- Nutritional-Metabolic: Evaluate the patient’s nutritional status, dietary habits, and ability to meet nutritional needs. Interventions may include providing dietary counseling, recommending dietary supplements, and assisting with meal planning.
- Elimination: Assess the patient’s elimination patterns, including bowel and urinary function. Interventions may include promoting regular bowel movements, managing incontinence, and addressing urinary tract infections.
- Activity-Exercise: Evaluate the patient’s activity level, exercise habits, and ability to perform daily activities. Interventions may include promoting physical activity, providing assistive devices, and recommending appropriate exercise programs.
- Sleep-Rest: Assess the patient’s sleep patterns, sleep quality, and ability to get restful sleep. Interventions may include establishing regular sleep-wake cycles, creating a conducive sleep environment, and recommending relaxation techniques.
- Cognitive-Perceptual: Evaluate the patient’s cognitive abilities, including memory, concentration, and problem-solving. Interventions may include providing cognitive stimulation, promoting memory aids, and addressing sensory impairments.
- Self-Perception-Self-Concept: Assess the patient’s self-perception, body image, and self-esteem. Interventions may include providing support and encouragement, promoting positive self-talk, and addressing negative body image.
- Role-Relationship: Evaluate the patient’s social relationships, family dynamics, and ability to fulfill roles. Interventions may include providing support for family caregivers, facilitating communication, and addressing relationship conflicts.
- Sexuality-Reproductive: Assess the patient’s sexual health, reproductive status, and ability to engage in satisfying sexual relationships. Interventions may include providing sexual health education, addressing sexual dysfunction, and supporting fertility treatments.
- Coping-Stress Tolerance: Evaluate the patient’s coping mechanisms, stress levels, and ability to manage stress. Interventions may include providing stress management techniques, promoting relaxation exercises, and addressing maladaptive coping mechanisms.
- Values-Beliefs: Assess the patient’s values, beliefs, and how they influence health behaviors. Interventions may include providing culturally sensitive care, respecting the patient’s religious practices, and addressing conflicts between beliefs and health practices.
Applications of Gordon Functional Health Patterns
Gordon’s Functional Health Patterns (FHPs) are extensively utilized in diverse healthcare settings to facilitate comprehensive patient assessments and individualized care planning. They provide a structured framework for gathering patient data, enabling healthcare professionals to identify potential health risks, promote health, and prevent disease.
FHPs contribute significantly to patient care by:
- Identifying health patterns and deviations from normal functioning
- Guiding patient education and counseling interventions
- Facilitating interdisciplinary collaboration among healthcare team members
- Evaluating patient outcomes and monitoring progress
Use of FHPs in Various Healthcare Settings
FHPs are widely applicable in various healthcare settings, including:
- Primary care: Assessing patients’ overall health status, identifying health risks, and developing preventive care plans
- Acute care: Evaluating patients’ functional abilities and providing necessary support during hospitalization or critical illness
- Long-term care: Monitoring patients’ health status, promoting independence, and preventing complications in long-term care facilities
- Mental health: Assessing patients’ mental and emotional health, identifying stressors, and developing coping mechanisms
- Public health: Identifying health trends, developing health promotion programs, and evaluating the effectiveness of public health interventions
Contribution to Comprehensive Patient Assessment and Care Planning
FHPs provide a comprehensive assessment of the patient’s health status by considering the following aspects:
- Health perception and management: Patient’s subjective perception of their health, health practices, and coping mechanisms
- Nutritional-metabolic: Patient’s nutritional status, eating habits, and metabolic processes
- Elimination: Patient’s bowel and urinary function, including patterns, regularity, and any difficulties
- Activity and exercise: Patient’s physical activity level, exercise habits, and any limitations
- Sleep and rest: Patient’s sleep patterns, quality of sleep, and any disturbances
- Cognitive-perceptual: Patient’s cognitive abilities, sensory perception, and communication skills
- Self-perception and self-concept: Patient’s perception of their own worth, body image, and self-esteem
- Role-relationship: Patient’s social roles, relationships, and support systems
- Sexuality and reproductive: Patient’s sexual health, reproductive history, and any concerns
- Coping and stress tolerance: Patient’s coping mechanisms, stress management techniques, and ability to adapt to challenges
- Values and beliefs: Patient’s personal values, beliefs, and cultural influences that impact their health
By considering these patterns, healthcare professionals gain a holistic understanding of the patient’s health, enabling them to develop individualized care plans that address the patient’s unique needs and circumstances.
Limitations and Considerations
While Gordon FHPs offer a comprehensive framework for health assessment, they are not without limitations and considerations.
Potential Limitations and Challenges
Potential limitations include:
- Subjectivity: FHPs rely on self-reporting, which can be influenced by personal biases, memory limitations, and social desirability.
- Time-consuming: Comprehensive FHP assessment requires significant time and effort from both the nurse and patient.
- Limited generalizability: FHPs were developed primarily for use in Western cultures and may not be applicable to all populations.
Ethical and Cultural Considerations
Ethical and cultural considerations are crucial in FHP assessment:
- Informed consent: Patients should be fully informed about the purpose and potential implications of the assessment.
- Cultural sensitivity: Nurses should be aware of and respect cultural differences in health beliefs and practices.
- Privacy and confidentiality: The patient’s privacy and the confidentiality of their information must be maintained.
By addressing these limitations and considerations, nurses can ensure that Gordon FHPs are used effectively and ethically to promote optimal patient care.