
Introduction
Electronic health records (EHRs) are digital versions of patients’ medical charts that contain their medical history, diagnoses, medications, and other important health information. They are a valuable tool for healthcare providers because they allow them to access patient information quickly and easily, which can lead to better care and more efficient use of resources.
Implementing EHRs can be a challenge, but the benefits of doing so outweigh the costs. EHRs can help healthcare providers improve the quality of care they provide, reduce costs, and improve patient satisfaction.
Benefits of EHRs
EHRs offer a number of benefits for healthcare providers and patients, including:
- Improved quality of care: EHRs can help healthcare providers improve the quality of care they provide by providing them with access to more complete and accurate patient information. This can lead to better diagnosis and treatment decisions, and can also help to prevent medical errors.
- Reduced costs: EHRs can help healthcare providers reduce costs by reducing the need for duplicate testing and paperwork. They can also help to improve efficiency by automating tasks and reducing the need for manual processes.
- Improved patient satisfaction: EHRs can help to improve patient satisfaction by providing patients with easier access to their medical records and by making it easier for them to communicate with their healthcare providers.
Challenges of Implementing EHRs
Implementing EHRs can be a challenge, but the benefits of doing so outweigh the costs. Some of the challenges associated with implementing EHRs include:
- Cost: EHRs can be expensive to purchase and implement. Healthcare providers need to carefully consider the costs and benefits of EHRs before making a decision about whether or not to implement them.
- Training: Healthcare providers need to be trained on how to use EHRs. This can be a time-consuming and expensive process.
- Data security: EHRs contain sensitive patient information, so it is important to ensure that they are secure. Healthcare providers need to implement strong security measures to protect patient data.
Types of EHR Programs
EHR programs vary in their capabilities and target audiences. Here are some common types available in the market:
Cloud-based EHRs
Cloud-based EHRs are hosted on remote servers and accessed through the internet. They offer flexibility, scalability, and lower upfront costs.
On-premise EHRs
On-premise EHRs are installed and maintained on the healthcare provider’s own servers. They provide greater control and customization but require significant upfront investment and ongoing maintenance.
Specialty-specific EHRs
Specialty-specific EHRs are designed for specific medical specialties, such as ophthalmology, dermatology, or orthopedics. They offer tailored features and workflows optimized for the needs of the specialty.
Ambulatory EHRs
Ambulatory EHRs are designed for outpatient clinics and physician offices. They focus on patient scheduling, medical history, and billing.
Hospital EHRs
Hospital EHRs are comprehensive systems designed for inpatient care. They include features for managing complex patient conditions, medication administration, and discharge planning.
Integrated EHRs
Integrated EHRs combine multiple EHR modules into a single platform. They offer a comprehensive view of patient data and streamline workflows across different departments.
Popular EHR Software
- Epic: Comprehensive EHR for hospitals and large healthcare systems.
- Cerner: Cloud-based EHR with a strong focus on interoperability.
- Allscripts: Ambulatory EHR with robust patient engagement tools.
- eClinicalWorks: Specialty-specific EHR with customizable templates.
- Athenahealth: Cloud-based EHR with a user-friendly interface.
Benefits of EHR Programs
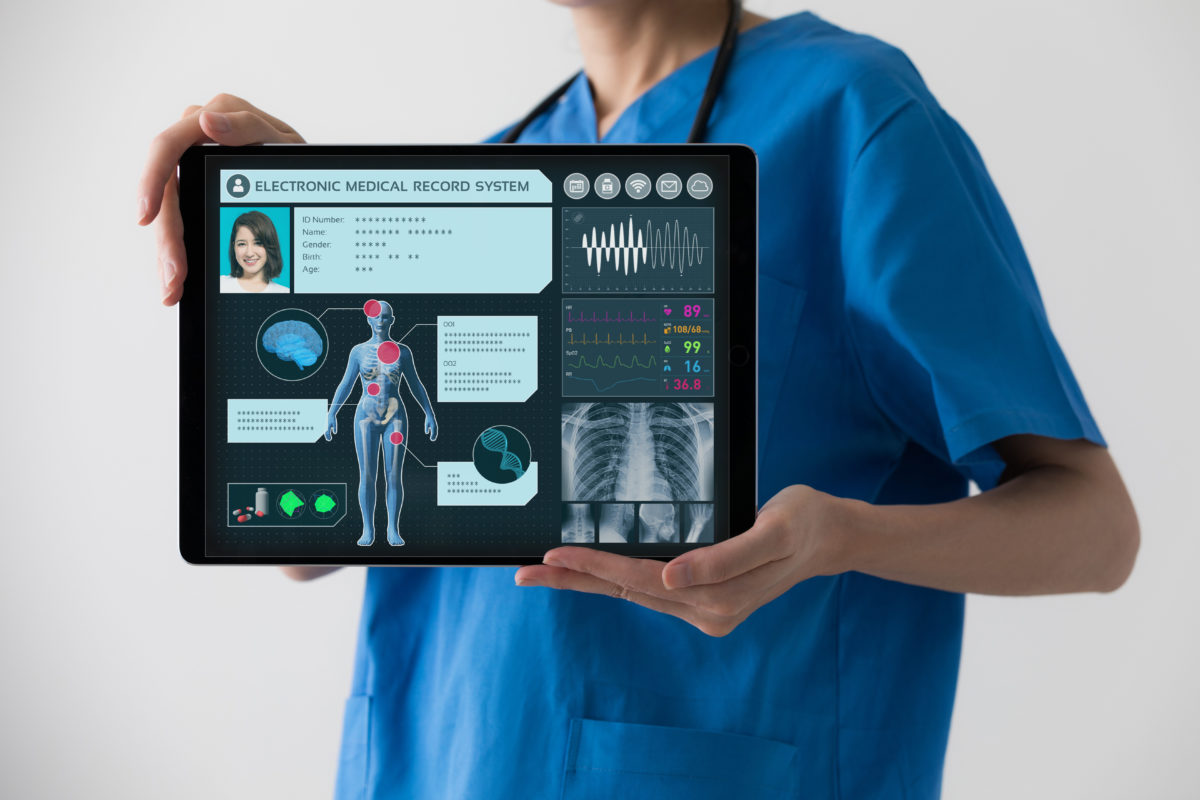
Electronic health records (EHRs) offer numerous advantages for healthcare providers and patients alike. They enhance patient care, streamline workflows, and significantly reduce costs.
Improved Patient Care
EHRs provide a comprehensive and up-to-date view of a patient’s medical history, making it easier for healthcare providers to make informed decisions about their care. They enable:
- Improved medication management, reducing medication errors and adverse drug reactions.
- Faster and more accurate diagnosis, as providers have access to a complete medical history.
- Enhanced patient engagement and self-management, empowering patients to take an active role in their healthcare.
Streamlined Workflows
EHRs automate many administrative tasks, freeing up healthcare providers to focus on patient care. They offer:
- Electronic prescribing, reducing errors and delays in medication fulfillment.
- Automated reminders for appointments, screenings, and vaccinations.
- Secure and efficient communication between providers, patients, and other healthcare professionals.
Reduced Costs
EHRs can significantly reduce healthcare costs by:
- Minimizing redundant testing and procedures due to better access to patient information.
- Improving coordination of care, reducing the need for expensive emergency room visits and hospitalizations.
- Reducing administrative costs through automation and streamlined workflows.
According to a study by the American Medical Association, EHRs have been shown to reduce healthcare costs by an average of 10-15%. Furthermore, a report by the Office of the National Coordinator for Health Information Technology found that EHRs can save up to $1,800 per patient per year.
Challenges of EHR Programs
While EHRs offer numerous benefits, implementing and using them can present several challenges.
One major challenge is interoperability, which refers to the ability of different EHR systems to communicate and exchange data seamlessly. Without interoperability, healthcare providers may struggle to access patient information from other systems, leading to fragmented care and potential patient safety risks.
Data Privacy
Another challenge is ensuring data privacy and security. EHRs contain sensitive patient information that must be protected from unauthorized access or breaches. Implementing robust cybersecurity measures is crucial to safeguard patient data and comply with regulatory requirements.
User Adoption
User adoption is another critical factor that can impact the success of EHR implementation. Healthcare professionals may resist using new EHR systems due to concerns about workflow disruption, training requirements, or perceived usability issues. Addressing these concerns and providing adequate training and support is essential for successful user adoption.
Future of EHR Programs
The future of EHR programs holds exciting possibilities, driven by technological advancements and the evolving healthcare landscape. Artificial intelligence (AI), machine learning (ML), and other cutting-edge technologies are transforming the way EHRs are designed and utilized.
AI and ML algorithms can analyze vast amounts of patient data, identify patterns, and provide insights that can enhance clinical decision-making. For instance, EHRs integrated with AI can predict patient outcomes, suggest personalized treatment plans, and flag potential complications early on.
Potential of Artificial Intelligence and Machine Learning
- Predictive analytics for disease risk assessment and early detection
- Personalized treatment recommendations based on individual patient characteristics
- Automated identification of medication interactions and adverse events
Innovative EHR Solutions
Innovative EHR solutions are emerging to address the challenges and capitalize on the opportunities presented by the future of healthcare. These solutions include:
- Cloud-based EHRs that provide secure, accessible data storage and seamless collaboration among healthcare providers
- Interoperable EHRs that facilitate the seamless exchange of patient information across different healthcare systems
- Patient-centric EHRs that empower patients with access to their own health records and the ability to engage in their care
Case Studies
Real-world EHR implementations have demonstrated their potential to revolutionize healthcare delivery. Case studies provide valuable insights into the challenges, lessons learned, and benefits of successful implementations.
Successful Implementations
One notable case study is the implementation of an EHR system at Intermountain Healthcare. The program streamlined patient data management, reducing medical errors and improving communication among healthcare providers. The result was a significant reduction in hospital readmissions and improved patient satisfaction.
Another success story is the adoption of EHRs at Kaiser Permanente. The system integrated patient records, enabling seamless care coordination across multiple locations. This led to improved chronic disease management, reduced emergency room visits, and enhanced patient engagement.
Challenges and Lessons Learned
EHR implementations are not without challenges. Interoperability issues, data security concerns, and user adoption difficulties are common hurdles. However, successful case studies highlight the importance of strong leadership, stakeholder engagement, and robust training programs to overcome these obstacles.
Improved Patient Care and Outcomes
EHRs have been shown to improve patient care and healthcare outcomes. They provide clinicians with real-time access to comprehensive patient information, facilitating more informed decision-making. Additionally, patient portals allow patients to view their medical records, communicate with providers, and manage their health. These features empower patients and contribute to improved self-management and adherence to treatment plans.
Best Practices for EHR Implementation
EHR implementation is a complex process that requires careful planning and execution. By following best practices, healthcare organizations can increase the likelihood of a successful implementation and achieve the full benefits of EHR technology.
Planning
The planning phase is critical to the success of an EHR implementation. During this phase, organizations should develop a clear implementation plan, including a timeline, budget, and resource allocation. They should also identify key stakeholders and develop a communication plan to keep everyone informed throughout the process.
Vendor Selection
Choosing the right EHR vendor is essential. Organizations should carefully evaluate vendors based on their experience, product offerings, and support services. They should also consider the vendor’s financial stability and ability to meet the organization’s specific needs.
Data Migration
Data migration is a complex and time-consuming process. Organizations should develop a data migration plan that includes a detailed inventory of all data to be migrated, as well as a plan for data validation and verification.
User Training
User training is essential for successful EHR adoption. Organizations should provide comprehensive training to all users, including physicians, nurses, and other staff members. Training should cover all aspects of the EHR system, from basic navigation to advanced clinical functionality.
Tips for Ensuring Successful EHR Adoption and Utilization
- Develop a clear implementation plan and timeline.
- Choose the right EHR vendor.
- Develop a comprehensive data migration plan.
- Provide comprehensive user training.
- Monitor EHR usage and make adjustments as needed.
- Get feedback from users and make improvements based on their feedback.
- Continuously evaluate the EHR system and make upgrades as needed.





