
- Understanding Insurance Credentialing for Mental Health Professionals
- The Credentialing Process
- Required Documentation and Information: How To Get Credentialed With Insurance Companies Mental Health
- Maintaining Credentials
- Navigating Insurance Reimbursement and Billing
- Resources and Support for Credentialing
- Last Word
- FAQ Corner
How to get credentialed with insurance companies mental health – Credentialing with insurance companies for mental health is the key to unlocking a world of possibilities for therapists, counselors, and other mental health professionals. It’s your ticket to a wider client base, more stable income, and the satisfaction of helping more people. But navigating the complex world of insurance credentialing can feel like a maze. This guide will break down the process, step by step, and provide all the information you need to get credentialed with insurance companies and start your journey towards success.
Imagine yourself, a licensed mental health professional, ready to help individuals navigate the ups and downs of life. But there’s a catch – most people rely on insurance to cover mental health services. This is where credentialing comes in. By getting credentialed, you’re essentially getting your “stamp of approval” from insurance companies, allowing you to bill for your services and get reimbursed. It’s a win-win situation – more patients can access your services, and you can build a thriving practice.
Understanding Insurance Credentialing for Mental Health Professionals
Insurance credentialing is the process of getting your mental health practice recognized by insurance companies. It’s like getting your official stamp of approval from the insurance world, allowing you to bill for your services and get paid for your expertise.
The Importance of Insurance Credentialing
Credentialing is a critical step for mental health professionals who want to work with clients who have insurance coverage. Without it, you’re limiting your potential client base and leaving money on the table. Being credentialed opens doors to a wider range of clients who can access mental health care through their insurance plans.
Benefits of Being Credentialed with Insurance Companies
There are numerous benefits to being credentialed with insurance companies. It’s like having a backstage pass to a world of possibilities. Here are some of the key advantages:
- Expanded Client Base: You can reach a broader range of clients who rely on insurance coverage for mental health care. Imagine a whole new audience knocking on your door, ready to benefit from your expertise.
- Increased Revenue: Getting paid for your services is crucial. Credentialing ensures that you receive reimbursement from insurance companies for the services you provide. You can say goodbye to those days of wondering where your next paycheck will come from.
- Streamlined Billing Process: Credentialing simplifies the billing process, allowing you to focus on what matters most: your clients. You can bid farewell to tedious paperwork and administrative headaches.
- Enhanced Professional Credibility: Being credentialed with insurance companies demonstrates your commitment to professional standards and quality care. It’s like having a gold star on your resume, signifying that you’re a true expert in your field.
Key Requirements for Credentialing in Mental Health
Credentialing isn’t just about filling out a few forms. There are specific requirements that you need to meet to demonstrate your qualifications. These include:
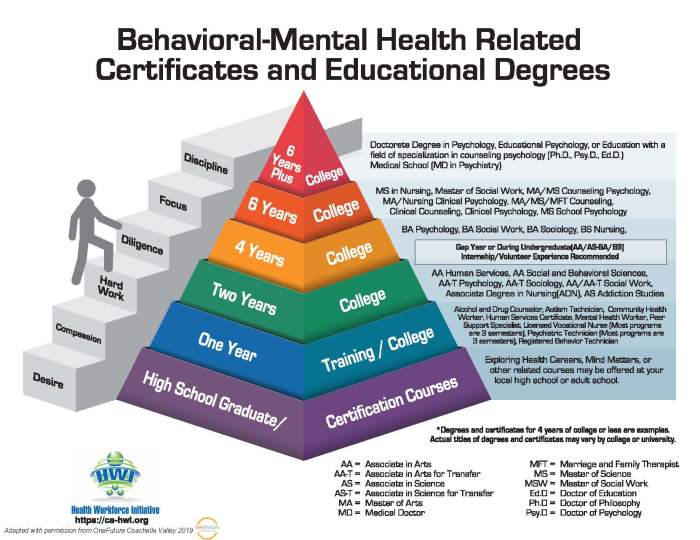
- Licensure and Certification: You need to have the necessary licenses and certifications in your state, proving that you’re a qualified mental health professional. Think of it as your official permission slip to practice.
- Professional Training and Experience: You need to demonstrate your training and experience in mental health, showcasing your expertise and ability to provide quality care. It’s like showing off your mental health superhero credentials.
- Background Check: Insurance companies conduct background checks to ensure the safety and well-being of their clients. It’s a standard procedure that helps maintain trust and security.
- Continuing Education: Staying up-to-date on the latest research and advancements in mental health is crucial. You need to demonstrate that you’re committed to continuous learning and professional growth. Think of it as constantly leveling up your mental health skills.
Types of Insurance Plans Mental Health Professionals Can Get Credentialed With, How to get credentialed with insurance companies mental health
There are different types of insurance plans that mental health professionals can get credentialed with, each with its own set of rules and requirements.
- Commercial Insurance Plans: These are plans offered by private insurance companies, like UnitedHealthcare, Anthem, and Aetna. They often have specific requirements for credentialing, such as participating in their provider networks.
- Government-Funded Insurance Plans: These plans are offered by government agencies, such as Medicare and Medicaid. They have their own sets of requirements for credentialing, often focusing on eligibility and service coverage.
- Managed Care Organizations (MCOs): These are health plans that manage the cost and quality of health care services. Credentialing with MCOs can provide access to a broader range of clients, but it also involves specific network requirements and utilization review processes.
The Credentialing Process
Alright, let’s dive into the nitty-gritty of getting credentialed with insurance companies, so you can start billing those sessions and get paid for your expertise. Think of it like a super-sized application process, but with a whole lot more paperwork. You’re basically saying, “Hey insurance companies, I’m legit! Let me treat your clients.”
Steps Involved in the Credentialing Process
This process is like a marathon, not a sprint. You’ll need to be patient and organized to get through it all. But don’t worry, we’ll break it down step by step.
- Gather Your Documents: This is like getting ready for a big game. You need all your gear. This includes your license, education credentials, and any other required paperwork. Think of it as your “mental health resume.” The insurance company will want to see everything to make sure you’re qualified.
- Complete the Application: This is where you’ll really put your paperwork skills to the test. Each insurance company has its own application, so get ready for some serious form-filling. It’s like a game of “find the right box.” Make sure you fill out everything accurately and completely, because even a tiny mistake can delay the process.
- Submit Your Application: You’ve got all your ducks in a row, and it’s time to send it off. Make sure you submit it electronically or by mail, depending on the insurance company’s instructions. This is like hitting “send” on that super important email. You’ve done your part, and now you’re waiting for a response.
- Verification Process: Now, the insurance company will take a look at your application and verify your credentials. This is like them checking your references. They’ll contact your licensing board, schools, and other organizations to make sure everything is legit. This step can take a while, so be patient.
- Provider Enrollment: If everything checks out, you’ll be enrolled as a provider. This is like getting your official “go-ahead” to treat patients. The insurance company will give you a provider number, which is your key to billing for services.
Required Documentation
Let’s talk about the paperwork. It’s a lot, but it’s all important. Think of it like a “mental health professional’s survival kit.”
- License: This is the most important document. It proves you’re legally qualified to practice. It’s like your driver’s license, but for mental health.
- Education Credentials: Your degrees and certificates show that you have the training to provide quality care. Think of it like your “mental health diploma.”
- Continuing Education Certificates: This shows that you’re keeping up with the latest trends in mental health. It’s like your “mental health membership card.”
- National Provider Identifier (NPI): This is a unique 10-digit number that identifies you as a healthcare provider. Think of it as your “mental health social security number.”
- Tax Identification Number (TIN): This is your business identification number, and it’s used for tax purposes. Think of it as your “mental health business license.”
- State-Specific Forms: Each state has its own requirements, so be sure to check what’s needed in your state. It’s like having your “mental health state ID.”
Timelines
Now, let’s talk about how long all this takes. Think of it like waiting for that big package to arrive. You want to know when to expect it, right?
- Initial Application: This part usually takes a few weeks to complete, depending on how quickly you can gather your documents and fill out the application. Think of it like a “sprint” at the beginning of the marathon.
- Verification Process: This is the real waiting game. It can take anywhere from a few weeks to a few months. Think of it like the “long haul” of the marathon.
- Provider Enrollment: Once your application is approved, you’ll be enrolled as a provider. This usually happens within a few weeks. Think of it like the “finish line” of the marathon.
Common Challenges Faced During the Credentialing Process
Alright, let’s talk about the bumps in the road. You’re not alone. Many mental health professionals face challenges during the credentialing process. Think of it like those unexpected potholes you encounter on your marathon route.
- Missing or Incomplete Documents: This is like forgetting your water bottle on a long run. You can’t go without it! Make sure you have all the required documents and that they’re filled out correctly.
- Incorrect Information: This is like taking a wrong turn on your marathon route. You’ll need to backtrack and make sure you’re on the right path. Double-check all your information before submitting your application.
- Delays in the Verification Process: This is like a roadblock on your marathon route. You can’t move forward until it’s cleared. Be patient and follow up with the insurance company if you experience delays.
- Communication Issues: This is like getting lost on your marathon route and not knowing how to get back on track. Keep in touch with the insurance company and ask questions if you’re unsure about anything.
Tips for Streamlining the Credentialing Process
Alright, let’s talk about some tips to make this process smoother. Think of it like having a “mental health credentialing coach” in your corner.
- Start Early: Don’t wait until the last minute to start the credentialing process. The earlier you start, the better. Think of it like starting your marathon training early.
- Be Organized: Keep all your documents in one place and create a checklist to track your progress. Think of it like having a “mental health credentialing binder.”
- Communicate Clearly: Ask questions if you’re unsure about anything. It’s better to be safe than sorry. Think of it like having a “mental health credentialing buddy.”
- Follow Up: Check in with the insurance company regularly to see the status of your application. Think of it like checking your marathon progress on your GPS watch.
- Use a Credentialing Service: There are companies that can help you with the credentialing process. Think of it like having a “mental health credentialing sherpa” to guide you through the mountains of paperwork.
Required Documentation and Information: How To Get Credentialed With Insurance Companies Mental Health
You’ve tackled the basics of insurance credentialing and the process itself. Now, let’s dive into the nitty-gritty: the documents and information you need to get your mental health practice rolling with insurance companies.
Think of it like this: you’re applying for a job, but instead of a resume and cover letter, you’re submitting your credentials to show you’re qualified to treat patients under their insurance plans.
Essential Documents and Information
Here’s a breakdown of the documents and information you’ll need to get credentialed, along with some tips to make the process smoother:
| Document Type | Description | Purpose | Required Format |
|---|---|---|---|
| Application for Provider Enrollment | This is your official application to join an insurance company’s network. | To provide the insurance company with your basic information and practice details. | Typically submitted online or via mail. Each insurance company will have its own specific application form. |
| National Provider Identifier (NPI) | Your unique identification number issued by the Centers for Medicare & Medicaid Services (CMS). | To identify you as a healthcare provider. | 10-digit number, available through the NPI Registry. |
| State License | Proof that you’re licensed to practice mental health in your state. | To demonstrate your legal ability to provide mental health services. | Issued by your state’s licensing board, typically in a digital or physical format. |
| Degrees and Certifications | Official copies of your degrees and certifications, such as your doctorate in psychology (PsyD or PhD) or your licensure as a Licensed Clinical Social Worker (LCSW). | To verify your education and qualifications. | Official transcripts or certificates issued by the awarding institutions. |
| Professional Liability Insurance (Malpractice Insurance) | Proof that you have insurance to cover potential legal claims arising from your practice. | To protect you and the insurance company from financial liability. | Certificate of insurance from your insurance carrier. |
| Tax Identification Number (TIN) | Your business’s federal tax identification number, also known as an Employer Identification Number (EIN). | To identify your practice for tax purposes. | 9-digit number issued by the IRS. |
| Bank Information | Your bank account details for receiving reimbursements from the insurance company. | To ensure smooth payment processing. | Bank name, account number, routing number. |
| Practice Information | Details about your practice, including your practice name, address, phone number, and website. | To provide patients with information about your practice. | Must be accurate and up-to-date. |
| Specialty Information | The specific areas of mental health you specialize in, such as anxiety, depression, or trauma. | To help the insurance company determine which patients you’re qualified to treat. | List of your areas of expertise. |
| Fee Schedule | A list of your fees for different services, such as individual therapy, group therapy, or medication management. | To determine the reimbursement rates for your services. | Clearly Artikeld with specific fees for each service. |
Remember, each insurance company has its own specific requirements, so be sure to review their provider manual or website carefully.
Maintaining Credentials

Think of your insurance credentials as your VIP pass to the world of mental health billing. Just like any good party, you need to make sure your pass is up-to-date and in good standing to keep the good times rolling. Maintaining your credentials is crucial for getting paid, and it’s an ongoing process that requires attention and effort.
Procedures for Maintaining Credentials
Keeping your credentials in good shape is like maintaining your social media presence – you need to stay active and engaged. Here’s how to do it:
- Stay informed about changes in credentialing requirements: Insurance companies are constantly updating their policies and procedures. Don’t get caught off guard – check for updates regularly. It’s like keeping your social media app updated to avoid glitches and enjoy the latest features.
- Submit required re-credentialing applications: Most insurance companies require you to re-credential every 1-3 years. Think of it as renewing your driver’s license – it’s essential to keep things running smoothly.
- Provide updated information as needed: Changes in your practice address, NPI number, or other key information can impact your credentialing status. Make sure to update your information promptly to avoid any delays in payments.
- Respond to credentialing audits and requests: Insurance companies may conduct audits to verify your credentials. Be responsive and provide any necessary documentation to avoid potential issues. It’s like responding to a friend’s request on social media – be prompt and helpful.
Common Credentialing Issues and How to Avoid Them
Credentialing issues are like those pesky social media trolls – they can pop up unexpectedly and cause a lot of frustration. Here are some common issues and how to avoid them:
- Incomplete or inaccurate application information: Double-check your application for errors before submitting it. It’s like proofreading your social media posts before hitting “enter” – a little extra effort can save you a lot of trouble.
- Missing or expired documentation: Make sure all required documentation is up-to-date and submitted on time. It’s like keeping your social media profile updated with current information – don’t let your credentials become outdated.
- Failure to respond to audits or requests: Be responsive to all credentialing inquiries. It’s like responding to a direct message on social media – don’t leave your credentials hanging.
- Lack of communication with insurance companies: Stay in touch with your insurance companies and keep them informed of any changes. It’s like keeping your social media connections active – maintain a good rapport with your insurance providers.
Resources and Tools for Managing Credentialing Requirements
Staying on top of credentialing can be a challenge, but there are tools and resources to help you navigate the process. It’s like having a handy social media management tool to keep your accounts organized and running smoothly.
- Credentialing software: There are software programs specifically designed to manage credentialing processes, track deadlines, and streamline communication with insurance companies. Think of it as a social media scheduling tool – it can save you time and effort.
- Credentialing consultants: If you need expert assistance, consider hiring a credentialing consultant. They can help you navigate the complex world of credentialing and ensure everything is in order. It’s like hiring a social media manager – they can take care of the details so you can focus on your practice.
- Professional organizations: Many professional organizations offer resources and support for credentialing. They can provide guidance, templates, and training to help you maintain your credentials. It’s like joining a social media group for mental health professionals – you can learn from others and get support.
Navigating Insurance Reimbursement and Billing

So, you’ve got your credentials, you’re seeing clients, and you’re ready to get paid. But how do you navigate the wild world of insurance billing? Don’t worry, it’s not as scary as it seems. We’ll break down the basics of insurance reimbursement for mental health services, dive into those mysterious billing codes, and give you some tips to make sure you get paid what you deserve.
Insurance Reimbursement Basics
Insurance reimbursement for mental health services is based on a fee-for-service model, meaning you get paid for each service you provide. The amount you’re paid depends on the client’s insurance plan and the specific service you’re providing. Most plans have a pre-determined rate for each service, known as the “allowed amount.” You’ll typically bill the insurance company for the full amount of the service, and they’ll pay you the allowed amount.
Billing Codes: The Secret Language of Mental Health Billing
Think of billing codes as the language of insurance. They tell the insurance company what service you provided and how much you’re charging for it. The most common billing code system used for mental health services is the Current Procedural Terminology (CPT) code system.
CPT codes are five-digit numbers that represent specific medical services.
For example, a CPT code for a 60-minute individual psychotherapy session is 90837. These codes are essential for accurate billing and reimbursement.
Common Billing Scenarios
Let’s look at some common scenarios you might encounter in your practice:
- Client has insurance: If a client has insurance, you’ll need to verify their coverage and get pre-authorization for services. This involves contacting the insurance company to confirm that the client’s plan covers mental health services and that they’re eligible for the services you plan to provide. Once pre-authorization is granted, you can proceed with billing the insurance company for the services you provide.
- Client has no insurance: If a client doesn’t have insurance, you’ll need to discuss payment options with them. You can offer a sliding scale, payment plans, or accept cash payments.
- Client has a high deductible: If a client has a high deductible, they may be responsible for a significant portion of the cost of their treatment. In this case, you’ll need to work with the client to determine how they can afford to pay for their services.
- Client is in a managed care network: If a client is in a managed care network, you’ll need to make sure you’re in-network with their insurance plan. If you’re not in-network, the client may have to pay a higher out-of-pocket cost for your services.
Tips for Optimizing Billing Processes
Here are some tips to streamline your billing process and get paid on time:
- Use a billing software: There are many billing software programs available that can help you track your billing and payments. This can save you time and reduce errors.
- Submit claims electronically: Electronic claims processing is faster and more efficient than paper claims. Most insurance companies now accept electronic claims.
- Follow up on claims: It’s important to follow up on claims that haven’t been paid within a reasonable timeframe. This will help ensure that you get paid for your services.
- Stay up-to-date on billing regulations: Insurance billing regulations are constantly changing. It’s important to stay up-to-date on these changes to ensure you’re billing correctly.
Resources and Support for Credentialing
Navigating the world of insurance credentialing can feel like trying to solve a Rubik’s Cube while juggling flaming torches. Don’t worry, you’re not alone! There are tons of resources and support systems out there to help you get credentialed and keep your practice running smoothly.
Key Resources and Organizations
These organizations are like your cheer squad, ready to guide you through the credentialing process. They provide valuable information, training, and support to mental health professionals.
- National Committee for Quality Assurance (NCQA): The NCQA is a non-profit organization that sets standards for healthcare quality. They offer resources for credentialing and re-credentialing, including a credentialing toolkit and a directory of credentialing organizations.
- American Psychological Association (APA): The APA offers a variety of resources for psychologists, including information on credentialing and billing. They also have a dedicated credentialing hotline for members.
- National Association of Social Workers (NASW): The NASW provides support and resources for social workers, including information on credentialing, licensing, and ethical practice.
- American Counseling Association (ACA): The ACA offers a range of resources for counselors, including information on credentialing, licensing, and professional development. They also have a dedicated credentialing department.
Online Platforms and Tools
The internet is a treasure trove of information, and there are several platforms and tools that can help you navigate the credentialing process.
- Credentialing Software: These platforms can streamline the credentialing process by automating tasks such as application submission, tracking, and reporting. Some popular options include:
- Availity: This platform offers a wide range of services for healthcare providers, including credentialing, billing, and claims management. Availity is used by many insurance companies, making it a convenient option for credentialing with multiple payers.
- EClinicalWorks: This software platform offers a variety of features for healthcare practices, including credentialing, billing, and electronic health records (EHR). EClinicalWorks has a dedicated credentialing module that can help you manage the entire process.
- PracticeSuite: This platform offers a comprehensive suite of tools for healthcare practices, including credentialing, billing, and practice management. PracticeSuite is designed to be user-friendly and can help you streamline your credentialing workflow.
- Online Forums and Communities: Joining online forums and communities can be a great way to connect with other mental health professionals and learn from their experiences. You can ask questions, share tips, and get support from peers who understand the challenges of credentialing. Some popular online forums include:
- PsychCentral: This website offers a forum for mental health professionals to discuss a variety of topics, including credentialing.
- Therapist Hub: This website offers a forum for therapists to connect with each other and share resources, including information on credentialing.
- LinkedIn: LinkedIn can be a valuable tool for connecting with other mental health professionals and finding mentorship opportunities. You can join groups related to credentialing and participate in discussions.
Benefits of Seeking Guidance from Credentialing Experts
Just like you wouldn’t try to fix your car engine without a mechanic, you shouldn’t tackle credentialing alone. Credentialing experts can help you navigate the complex process and avoid common pitfalls.
- Specialized Knowledge: Credentialing experts have a deep understanding of the regulations, requirements, and best practices for credentialing with insurance companies. They can help you ensure your application is complete and accurate, increasing your chances of approval.
- Time Savings: Credentialing can be a time-consuming process, and seeking guidance from experts can save you valuable time and effort. They can handle the paperwork, track deadlines, and communicate with insurance companies on your behalf.
- Reduced Stress: Credentialing can be a stressful process, especially if you’re unfamiliar with the requirements. Working with a credentialing expert can help you reduce stress and focus on your practice.
Mentorship Programs and Professional Development Opportunities
Finding a mentor can be like having a personal cheerleader in your corner, guiding you through the credentialing journey. Look for mentorship programs and professional development opportunities that focus on credentialing.
- Mentorship Programs: Many professional organizations offer mentorship programs for mental health professionals. These programs can connect you with experienced professionals who can provide guidance and support throughout the credentialing process.
- American Psychological Association (APA): The APA offers a mentorship program for psychologists, which can help you connect with a mentor who can provide guidance and support on credentialing and other aspects of your career.
- National Association of Social Workers (NASW): The NASW offers a mentorship program for social workers, which can help you connect with a mentor who can provide guidance and support on credentialing and other aspects of your career.
- Professional Development Workshops: Many organizations offer workshops and training sessions on credentialing. These workshops can provide you with valuable information on the process, requirements, and best practices.
- National Committee for Quality Assurance (NCQA): The NCQA offers workshops and training sessions on credentialing, including a comprehensive credentialing toolkit.
- American Counseling Association (ACA): The ACA offers workshops and training sessions on credentialing, billing, and other aspects of running a successful counseling practice.
Last Word
The journey to becoming credentialed with insurance companies may seem daunting, but it’s a crucial step for any mental health professional looking to expand their reach and impact. By understanding the process, gathering the necessary documentation, and staying organized, you can successfully navigate the path to credentialing and open doors to a fulfilling career. Remember, it’s about helping people in need, and with the right guidance, you can achieve your goals and make a real difference in the lives of others.
FAQ Corner
What are the most common insurance plans that mental health professionals get credentialed with?
The most common insurance plans for mental health professionals include major players like Blue Cross Blue Shield, UnitedHealthcare, Aetna, Cigna, and Humana. You can also consider smaller regional or state-specific plans depending on your practice’s location and target clientele.
How long does the credentialing process typically take?
The credentialing process can take anywhere from a few months to a year, depending on the complexity of your application, the insurance company’s processing time, and any potential delays due to missing information or documentation.
What are some common mistakes to avoid during the credentialing process?
Some common mistakes to avoid include submitting incomplete or inaccurate information, failing to meet deadlines, and not following up regularly with the insurance company. It’s also important to maintain accurate and up-to-date contact information with the insurance company.
What are some resources for mental health professionals seeking credentialing support?
Several resources are available for mental health professionals seeking credentialing support, including the National Committee for Quality Assurance (NCQA), the American Psychological Association (APA), and the American Counseling Association (ACA). These organizations offer guidance, training, and resources to navigate the credentialing process.





